In this article one of our knee consultants, Mr Rahul Patel goes into detail about two of the most common knee injuries. Find out more about Rahul and how to book an appointment.
Knee Injuries
Two of the most common knee injuries, associated with what medical professionals describe as cutting and pivoting sports, are the meniscal tear and anterior cruciate ligament (ACL) rupture. Often, the two co-exist. In this short article, I want to bring you up to speed with current treatment concepts and options.
Meniscal Tear
What is the meniscus?
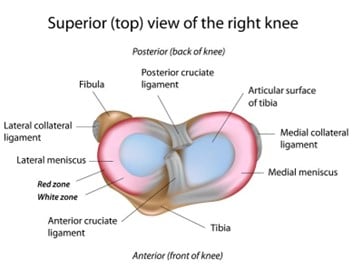
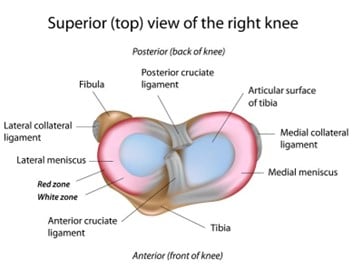
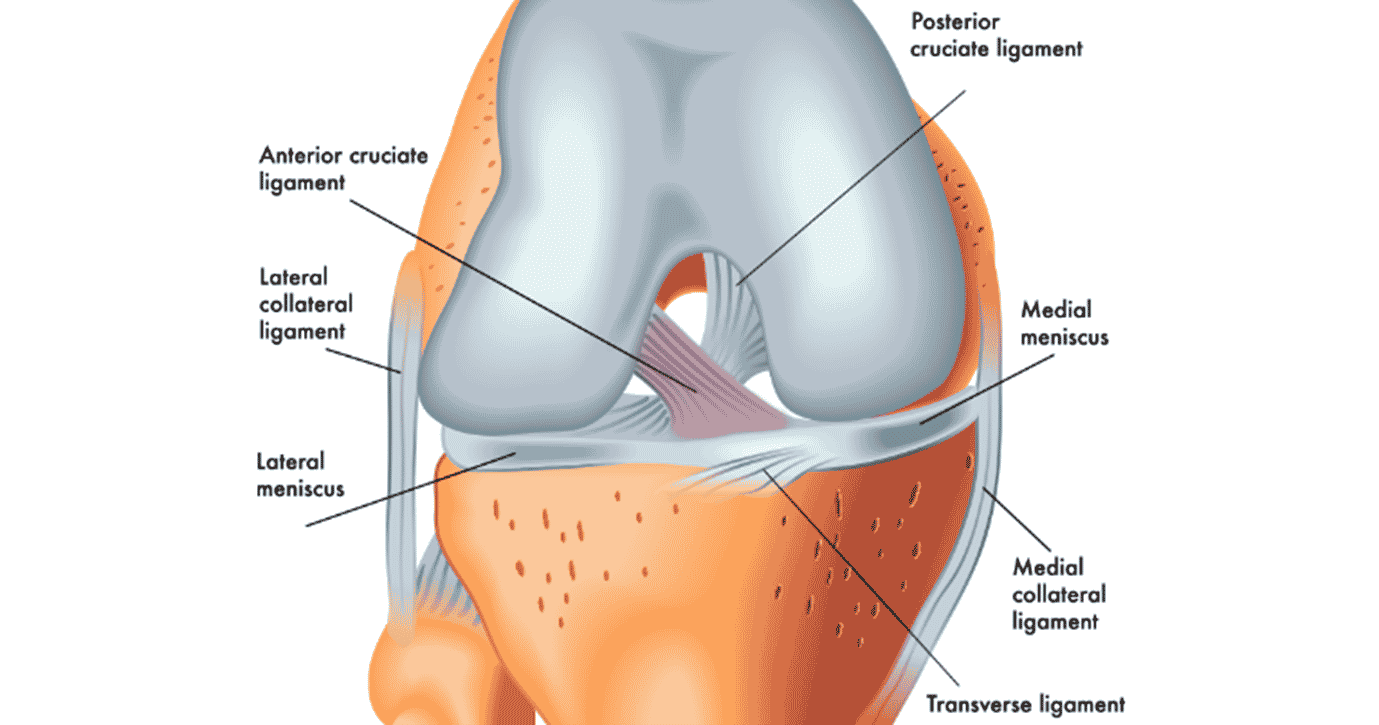
The meniscus is a specialised C-shaped disc of cartilage (fibrocartilage actually) that sits in between the two main bones that make up the knee joint, the femur and tibia. We have two, one on each side of the joint (medial and lateral) and their job is to distribute the load imparted across the joint evenly.
What is a meniscal tear?
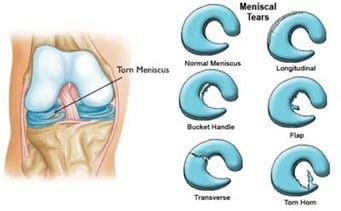
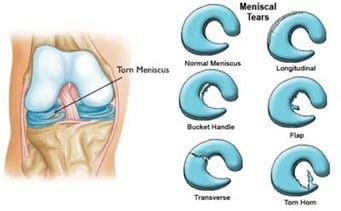
The meniscus is elastic and designed to be able to load distribute and cope with the combined forces placed upon it efficiently, but there are instances when the force and pressure on the meniscus are injurious, classically an awkward, violent twist of the knee, which results in a meniscal tear. In addition, as we age, the meniscus naturally becomes more vulnerable to this type of injury, and more innocuous mechanisms of injury can result in a (degenerate) tear.
Why all the fuss? Can’t it heal itself?
Unfortunately, on the whole, the meniscus can’t heal itself when torn. The tear persists and can cause symptoms of pain (often localised to the side of the knee in which the meniscus is torn), intermittent or persistent swelling and mechanical symptoms, such as clicking and catching. In larger tears, the knee can sometimes become temporarily stuck (locked) in a position which can be very disconcerting.
Common symptoms of a meniscal tear:
- Pain in the knee joint; usually on the out or inside, or the back of the knee.
- Swelling
- Stiffness
- Catching, locking, or clicking
- Difficulty fully straightening or bending the knee
- A feeling of weakness in the knee
So what shall I do?
Acutely, the adage of rest, ice, compression, and elevation is appropriate. Add to that, over-the-counter analgesics such as Paracetamol and Ibuprofen. You should seek medical attention to confirm the injury and to exclude more serious injuries such as fractures and ligament injuries. If the knee is locked, then a more urgent assessment is advised. The swelling and pain usually settle within 2-4 weeks but frequently, incompletely. If you can access a physiotherapist, they can help reduce swelling and recover range of motion to help you function day to day, but persisting symptoms suggest an orthopaedic knee specialist assessment is required.
Should I wear a brace?
Meniscal tears are not an indication of a brace per se. A simple knee sleeve (neoprene) can be helpful though in restoring confidence in the knee.

Should I have an MRI scan?
Your orthopaedic knee consultant will likely request an MRI scan. You can obtain one before your consultation, but it may be easier for your surgeon to organise it for you.

Will I need surgery?
Not necessarily is the short answer! Because the meniscus has such poor inherent healing capacity, the likelihood of surgery for a torn meniscus is moderate. Physiotherapy and time can result in manageable symptomology, especially for the more sedentary individual, but all too often a return to full activity, especially sports, is hindered. The good news is that meniscal tears can be dealt with using keyhole (arthroscopic) surgery which allows the meniscal surgery to be day case surgery and the recovery to be rapid. Full discussion with your orthopaedic knee surgeon and physiotherapist is advised.
London Bridge Orthopaedics work with several highly skilled and experienced Physiotherapist, and we will ensure that you are referred to someone who is best suited to your individual needs.
What happens during surgery?
Because the meniscal tear can’t heal, the traditional solution is to remove (resect) the torn fragment. This works very well in the majority of cases; allowing a swift return to work and sport, following complete resolution of symptoms. The trend in the last decade has been to try and save meniscal tissue if possible, by repairing (stitching) the tear and hoping that it will heal. Meniscal repair is more successful if the tear is near the outer edge of the meniscus where there is some blood supply and if the meniscal tissue is of good quality. It is also more likely to succeed in younger individuals (under the age of 40yrs). It is generally impossible to tell if a tear can be repaired or not from an MRI scan and is usually a decision the surgeon makes during the arthroscopy based on numerous factors, including the general state of the knee joint, types of sport you play and the level, as well as age and tear characteristics. Meniscal repair changes the rehabilitation and return to sports time from surgery significantly and therefore full discussion with your orthopaedic surgeon on this topic is advised.
What if I don’t have surgery and leave my tear alone?
This is certainly an option of treatment, particularly if your symptoms are manageable, and if you have a degenerate tear which doesn’t bother you much. However, you should know that an untreated meniscal tear, despite not causing much pain and swelling, can slowly abrade the surface of the joint leading to premature localised early osteoarthritis (loss of cartilage from the surface of the joint). This risk may be greater than the risk of developing arthritis following keyhole removal of some of the meniscus depending on your age. Your specialist knee surgeon can provide more detail on this. Thus, if you are young and have an acute, non-degenerate, continually symptomatic tear, then you should consider surgical options.
If you are older and have associated arthritis, which has been painful in the past, treating the meniscal tear (degenerate) is not likely to result in full symptom relief because arthritis cannot be reversed by keyhole surgery. Other options of treatment should be discussed with your orthopaedic surgeon in this case.
What’s new in meniscal surgery?
Meniscal resection or repair are the two main first-line treatments for a meniscal tear. If successful (they carry high success rates), they result in symptom-free function at high activity levels. Losing meniscus, especially at a young age, may confer a slightly higher overall risk of developing arthritis compared with not losing meniscus. Thus new technology centres on meniscal preservation and replacement (transplant). Repair techniques are sufficiently advanced to be reproducible and attention has turned to enhancing the healing response of the native meniscus and biological solutions to replacing the meniscus if it cannot be preserved. The latter is called a meniscal transplant where a full donated meniscus, which is accurately sized for the recipient, is surgically transplanted into the knee. This type of surgery has actually been carried out very successfully for decades and I offer this procedure to my suitable patients.
Anterior cruciate ligament (ACL) rupture
What is the ACL?
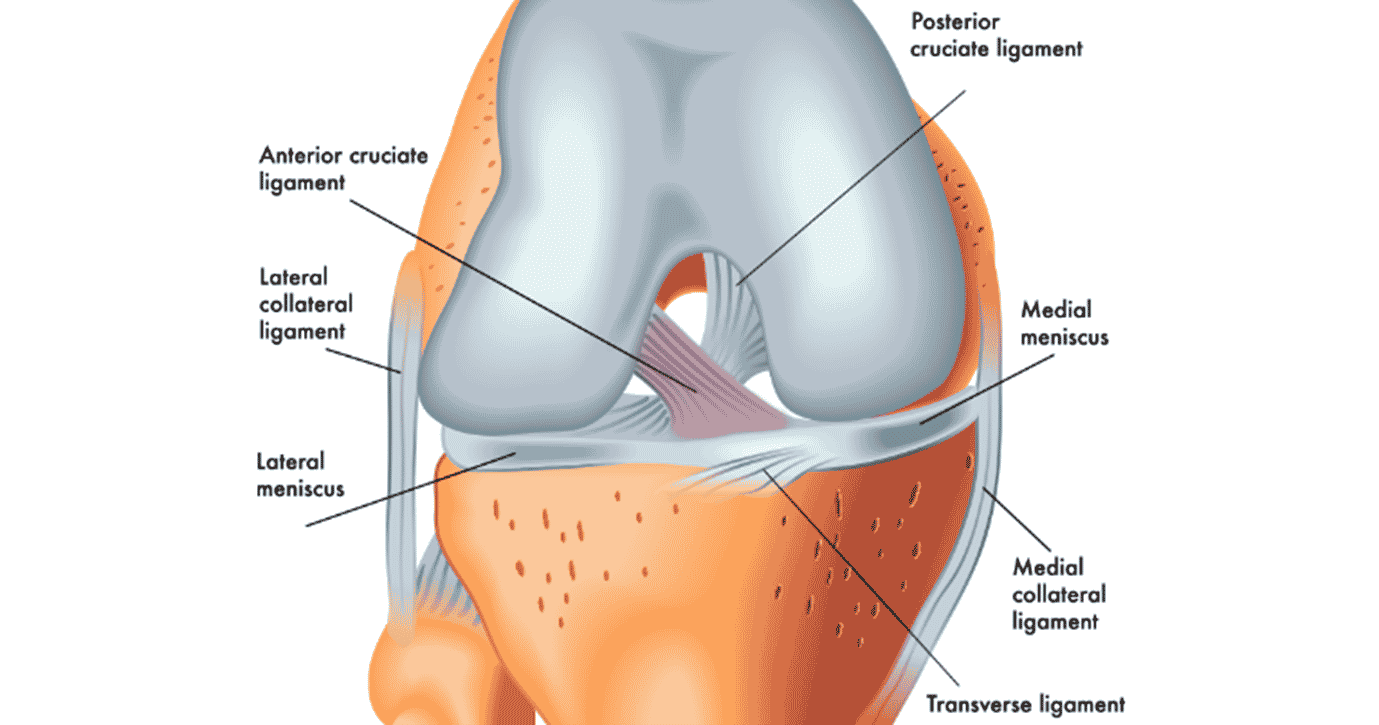
The ACL is a short, but vital ligament found in the middle of the knee. It is one of two cruciate ligaments (cf. posterior cruciate ligament) but is injured far more frequently than its partner. It runs between the femur and the tibia in an oblique direction. Its role is to confer stability to the knee, particularly with cutting and pivoting movements e.g. changing direction quickly or side-to-side movements.
What is ACL rupture?
This is when the ACL is torn (usually completely) as a result of injurious force (commonly twisting) placed across the knee. Interestingly, the majority of ACL injuries are non-contact injuries e.g., an awkward landing after jumping. Some sports have a greater association with ACL injuries such as football, rugby, skiing, netball, basketball, and martial arts, but the injury can occur in non-athletic scenarios as well! Usually, the injured person feels a painful ‘pop’ from the knee at the time of injury and cannot play. There may be immediate swelling of the knee but not always.
Common symptoms of an ACL tear:
- A loud popping sound or sensation in the knee
- Severe pain and inability to continue the activity
- Rapid swelling and bruising
- Loss of knee movement
- A feeling of instability or the knee giving way
- Difficulty weight-bearing

So, what shall I do?
Rest, ice, compression, elevation, and analgesia are sound acute self-treatment. It is important to seek medical assessment to exclude fracture (usually via an X-ray). The examining doctor may have a high index of suspicion of an ACL injury and should refer you to an orthopaedic specialist for further assessment. ACL ruptures can occur as part of combined injuries involving other ligaments around the knee and the menisci (see above); thus, early specialist opinion is recommended. Swelling and pain usually settle within 2-4 weeks and many individuals can walk well and function day to day with an ACL rupture. The key persisting symptom is instability – a feeling that the knee may give way (or does give way) with sudden changes in direction whilst walking or sideways movements. A further apprehension to return to any sporting activity due to poor confidence in the knee is also suggestive of ACL rupture. Seeing a physiotherapist early will help return to day-to-day function and is recommended. MRI scans are requested routinely to confirm the diagnosis of ACL rupture.
Can it heal itself?
The ACL cannot heal or repair itself and thus once ruptured, often results in persistent instability and apprehension to return to full sporting activity.
Does everyone with ACL rupture need surgery?
Depending on an individual’s level of activity and sports participation, ACL reconstruction surgery can be debated. Some can rehabilitate under physiotherapists’ guidance, to a point where the knee seldom gives way during the activities that they participate in; this applies mostly to sedentary individuals. The majority of people who wish to remain active at the same level as pre-injury will require surgery to reconstruct the ACL. There is no theoretical age limit to ACL reconstruction, rather activity level requirements and general status of the knee form the major determinants of whether surgery can be considered or not. Full discussion with your orthopaedic surgeon is advised, particularly about the risks of not having the ACL reconstructed. Recent evidence suggests that ACL deficient knees carry a higher risk of damaging other structures within the knee due to instability episodes e.g., meniscus. It is this risk of meniscal damage, that then increases the risk of developing earlier arthritis.
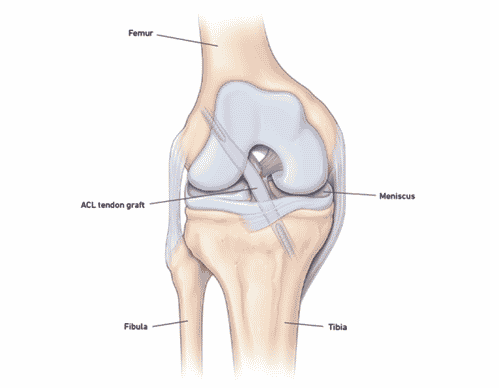
What does the surgery involve?
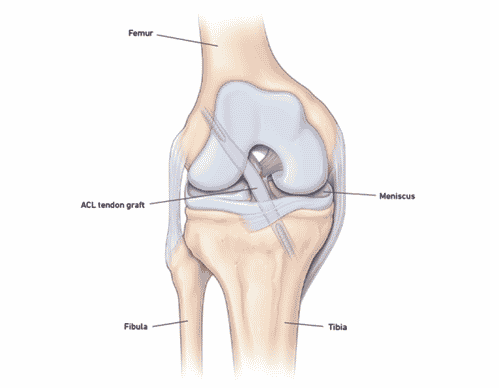
If you have chosen to have ACL reconstruction surgery, your specialist knee surgeon will discuss in detail how this is done in his/her hands. Surgeons usually utilise tissue from elsewhere around your knee to reconstruct the ACL e.g., hamstring tendons, patella tendon, quadriceps tendon; to be clear, the native ACL (ruptured) is removed, and a new ligament is fixed in its place using special devices.
ACL reconstruction surgery is very common and technology in this area of sports orthopaedic surgery is rapidly evolving and improving. It is keyhole (arthroscopic) surgery and can be carried out as a day case. Concurrent injuries to the meniscus or surface of the joint (chondral injury) can be treated at the same time. In fact, meniscal repair and cartilage stimulation techniques have been shown to be more successful when they are carried out concomitantly with an ACL reconstruction. After surgery, you will require crutches for 2-4 weeks and should start a formal physiotherapy program approximately 2 weeks after surgery. Your orthopaedic surgeon will discuss surgery and post-surgery management in detail with you.
Is ACL reconstruction successful?
ACL reconstruction is one of the most successful orthopaedic procedures in terms of returning individuals to high-level activity. Success is heavily dependent on good, structured rehabilitation, and patient compliance is central to achieving good outcomes. Most ACL rehabilitation programs run for approximately 6-9 months and return to contact sports is not advised before this time or until advised by your orthopaedic surgeon and physiotherapist. It takes time to build muscle and develop neuromuscular pathways, both negatively affected by the ACL rupture and subsequent surgery. Moreover, the reconstructed ACL (often referred to as the ACL graft) takes time to heal to you, a process that surgeons cannot currently influence predictably.
Your consultant at London Bridge Orthopaedics will ensure that you are referred to a Physiotherapist who can tailor your rehabilitation programme to exactly suit your individual needs. We work with some of the most highly experienced physiotherapists in London.
What’s new in ACL reconstruction surgery?
Newer ways to reconstruct the ACL are constantly being developed. It is the surgeons’ role to exercise caution in this respect and choose methods which are tried and tested rather than experimental. If your surgeon intends to use a new device or technique, he/she should provide a full explanation on the subject, including available evidence so that you are fully informed before you proceed with surgery. Similarly, new rehabilitation techniques are being used, and your physiotherapist will be able to discuss these with you in full.
The sports pages of newspapers recount the plight of our top-flight sports people and knee injuries, in particular, are common. We often read that our home-grown athletes have undergone specialist knee surgery to remedy the problem, maybe even abroad, and the story is often told in a manner which implies that the treatment these individuals receive, is only available to the elite. Well, it’s not the case. The exact same treatment is available to all, in the UK, from surgeons and physiotherapists with all the same skills and equipment. Elite-level treatment for all!
At London Bridge Orthopaedics we have three exceptional knee consultants. If you are a new patient and would like to book, please call our new patient booking line on 020 7692 0675 or visit our website and complete an appointment request.