Osteoarthritis (OA) of the elbow is a degenerative joint condition that causes the cartilage within the elbow joint to gradually wear away. Although less common than OA in the knees or hips, it can significantly impact daily function and quality of life—especially in individuals who rely on arm strength or mobility for work or sport.

Elbow OA leads to joint pain, stiffness, swelling, and mechanical symptoms such as catching or locking. It can affect the ulnohumeral joint (between the humerus and ulna) or the radiocapitellar joint (between the radius and humerus), or both. Although OA is more common in older adults, it can also affect younger people—particularly manual labourers and athletes with a history of trauma or repetitive use.
While OA cannot be cured, a combination of targeted treatments can relieve symptoms and maintain or improve elbow function.
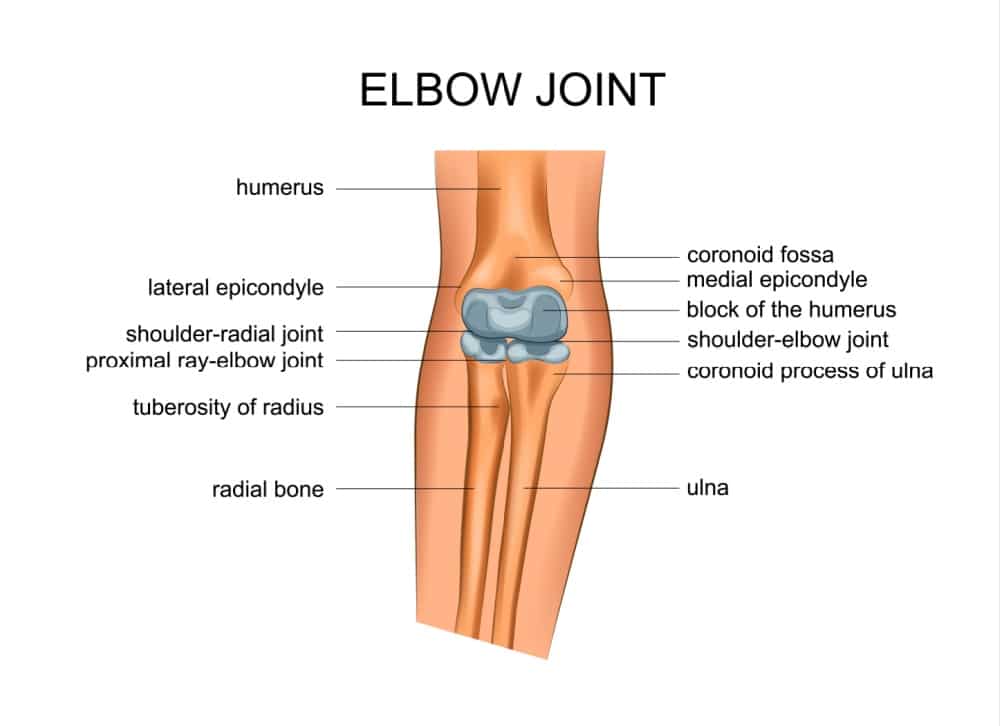
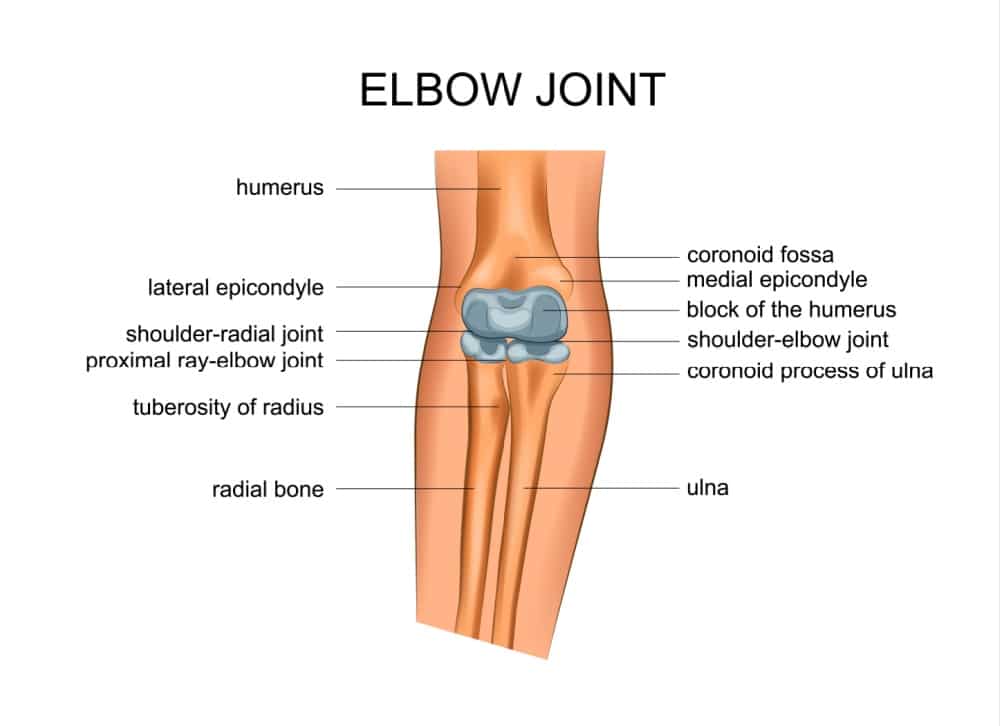
Anatomy of the Elbow
The elbow is a hinge-type synovial joint composed of three bones:
- Humerus (upper arm bone)
- Ulna (inner forearm bone)
- Radius (outer forearm bone)
These bones form two main articulations:
- The ulnohumeral joint, which allows bending and straightening of the elbow
- The radiocapitellar joint, which assists with forearm rotation
Articular cartilage lines the joint surfaces, enabling smooth, friction-free movement. Surrounding the joint are ligaments, tendons, muscles, and a synovial membrane that produces lubricating fluid. In OA, the cartilage thins and wears away, resulting in bone-on-bone contact, inflammation, and the formation of osteophytes (bony spurs).
Causes of Elbow OA
Elbow OA may be primary (age-related) or secondary (due to previous injury or joint disease).
Primary OA
- Occurs as part of the natural ageing process, typically in those aged 50 and above.
- Often seen in individuals with a long history of heavy manual work, repetitive lifting, or sports that place high stress on the elbow.
Secondary OA
Develops after trauma such as:
- Elbow dislocation
- Fractures involving the joint surface
- Post-surgical changes
May also follow inflammatory joint conditions (e.g., rheumatoid arthritis or gout)
Seen in younger individuals, particularly men, who have been active in jobs or sports requiring repetitive arm loading
Activities and Mechanisms of Injury
OA of the elbow is more common in:
- Manual labourers (e.g., builders, mechanics, electricians)
- Throwing athletes (e.g., cricket bowlers, baseball pitchers, javelin throwers)
- Weightlifters and strength trainers
- Martial artists or sports involving impact through the upper limbs (e.g., boxing, judo)
Mechanically, the repetitive extension-flexion cycle under load, especially with rotation (as in throwing or drilling), can lead to progressive cartilage wear and microtrauma over time.
Symptoms of Elbow OA
Elbow OA often develops gradually over several years. Symptoms may be mild at first and progress slowly with increasing use or age.
Pain
- Aching or sharp pain, typically felt on the inside (medial) or back (posterior) of the elbow
- Worsens with activity, especially gripping, lifting, or pushing motions
- May become more persistent and occur at rest in advanced cases
Stiffness
- Reduced ability to fully straighten (extend) or bend (flex) the elbow
- Morning stiffness or stiffness after inactivity is common
Clicking, Locking, or Catching
- Mechanical symptoms caused by loose bodies or osteophytes in the joint
- May result in sudden blocks to movement or a sensation of the joint “grinding”
Swelling and Joint Thickening
- Occasional swelling after use
- Over time, the joint may appear enlarged or deformed due to bony overgrowth
Weakness and Loss of Function
- Reduced grip strength and endurance
- Difficulty with tasks such as carrying heavy items, pushing doors open, or using tools
Diagnosis of Elbow OA
Diagnosis of elbow OA begins with a full clinical evaluation, including discussion of:
- Symptoms
- Activity levels and work demands
- Previous elbow injuries or surgeries
Physical Examination
- Joint movement will be assessed, especially any loss of extension
- Signs of instability, crepitus (grinding), or pain during range-of-motion testing
Imaging
- X-rays: Show typical changes such as joint space narrowing, osteophyte formation, and loose bodies
- MRI or CT scan: May be required for surgical planning or to assess associated conditions such as cartilage defects or impingement
Differential Diagnosis
Other conditions may mimic or coexist with elbow OA:
- Elbow tendinopathies (e.g., tennis elbow or golfer’s elbow)
- Loose bodies without generalised OA
- Osteochondritis dissecans
- Post-traumatic stiffness or arthritis
- Nerve compression syndromes (e.g., ulnar nerve entrapment)
Treatment Options
Non-Surgical Treatment
Most patients can manage elbow OA symptoms with non-operative treatments:
- Activity modification: Reducing repetitive strain and adjusting techniques or tools at work
- Physiotherapy: To maintain range of motion, reduce stiffness, and strengthen the surrounding musculature
- Pain relief: NSAIDs or paracetamol as needed
- Elbow braces: Can help stabilise the joint and reduce strain
- Corticosteroid injections: Provide temporary relief during flare-ups by reducing inflammation
- Hyaluronic acid injections: Occasionally used in early OA for lubrication and symptom control
Surgical Treatment
Surgery may be recommended when symptoms significantly interfere with daily life, and non-operative measures are no longer effective.
Surgical Options
Arthroscopic Debridement (Keyhole Surgery)
Used for early or moderate OA. Loose fragments, inflamed tissue, and bone spurs are removed using a camera and small instruments. This improves motion and reduces pain.
Open Debridement
In more advanced cases, open surgery may be required to remove larger bone spurs and loose bodies that are inaccessible arthroscopically.
Elbow Interposition Arthroplasty
A soft tissue graft is inserted between joint surfaces for younger patients with arthritis who are not yet suitable for joint replacement.
Total Elbow Replacement (Arthroplasty)
Used in severe OA, particularly in elderly or low-demand patients. The worn joint is replaced with a metal and plastic prosthesis to restore movement and reduce pain.
Who Benefits from Surgery?
Surgical treatment may be appropriate for:
- Patients with significant pain, particularly if it interferes with work or sleep
- Loss of functional elbow range, especially extension block
- Persistent mechanical symptoms (locking, catching) from osteophytes or loose bodies
- Severe joint degeneration confirmed by imaging
Outcomes
- Arthroscopic or open debridement often provides good symptom relief and functional improvement, especially in early-stage disease.
- Elbow replacement offers excellent pain relief and functional restoration but is generally reserved for older adults or low-impact use due to implant lifespan limitations.
- Post-operative rehabilitation is essential and tailored to the procedure, typically involving physiotherapy over 6–12 weeks.
FAQs
Can elbow osteoarthritis be prevented?
While it can’t always be prevented, minimising repetitive elbow stress, using ergonomic tools, and treating injuries promptly can help reduce risk.
How long is recovery after elbow surgery?
It depends on the procedure. Arthroscopy may require a few weeks, while total elbow replacement may need several months of rehabilitation.
Can I still work with elbow OA?
Yes, many people continue working with elbow OA by modifying tasks, using supports, and managing symptoms with physiotherapy and medication.
Does elbow OA always need surgery?
No. Many cases are successfully managed non-surgically. Surgery is only considered if pain or stiffness severely affects function.
Will I regain full movement after elbow surgery?
While full motion may not always be restored, most patients regain a functional range that allows daily activities without pain.