As temperatures drop and winter sets in, many patients tell me their shoulder stiffness and pain feels worse. It’s a common belief, and understandably, some assume this is where the term “frozen shoulder” comes from.
But while colder weather may heighten pain sensitivity, the condition itself has nothing to do with climate.
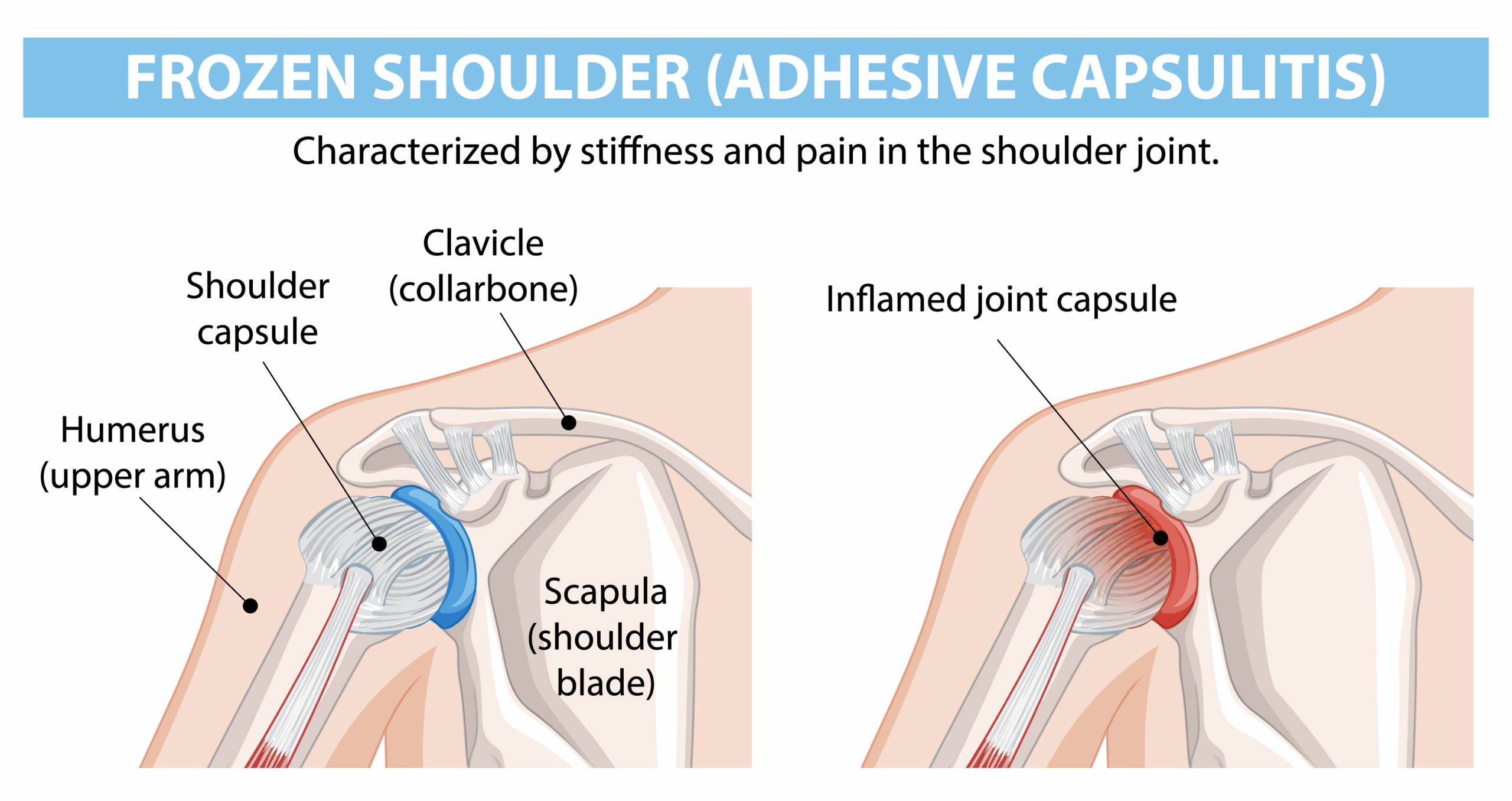
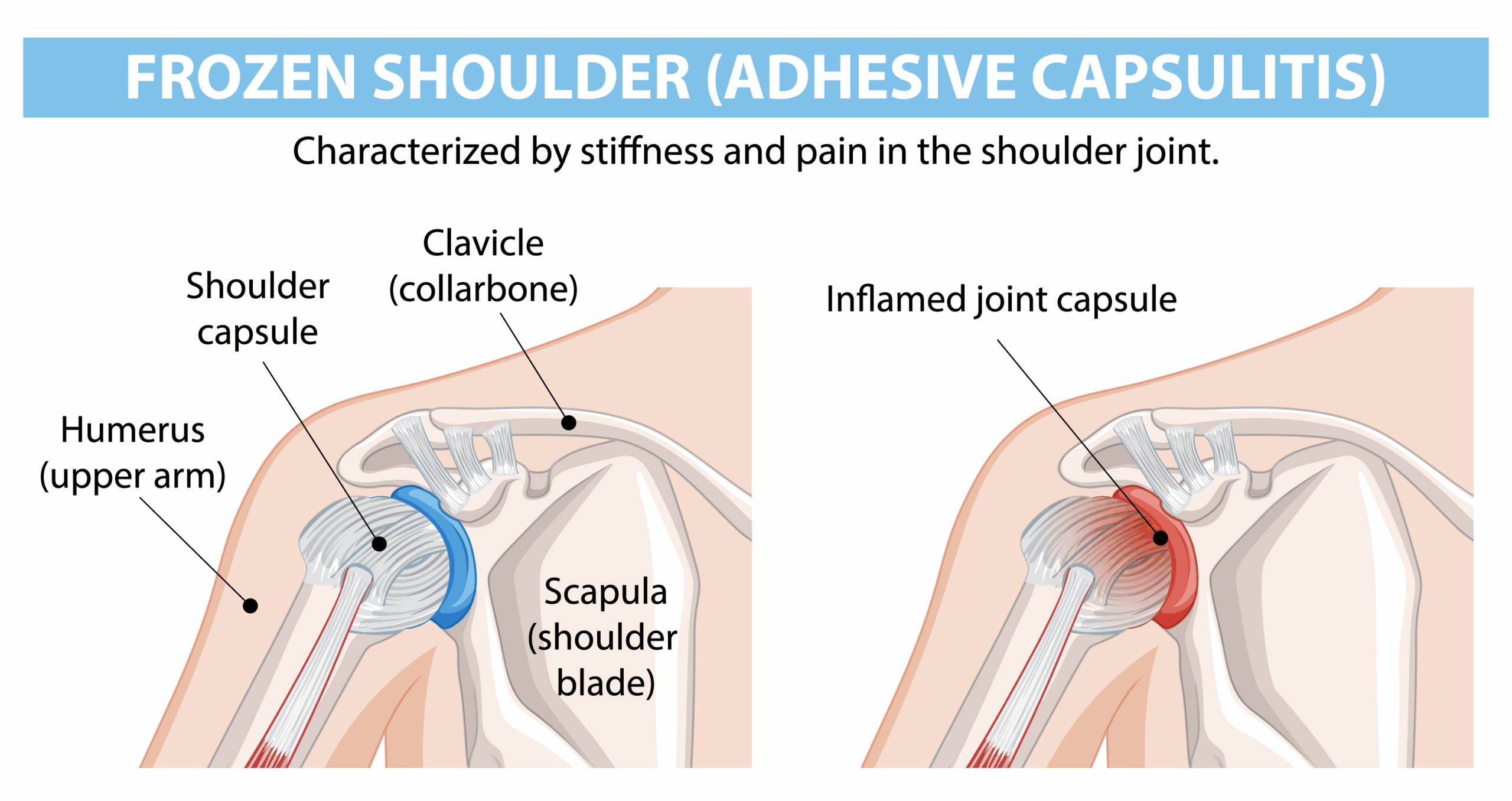
Frozen shoulder, medically known as adhesive capsulitis, is a condition involving inflammation, thickening and contracture of the shoulder capsule, leading to progressive stiffness and pain.
It has a very distinct natural history and clinical presentation, regardless of season. However, winter often acts as a catalyst for people to finally seek help, as activities such as putting on a coat, driving, or sleeping become increasingly difficult.
So, is cold weather really to blame? And what can be done to help?
Key Takeaways
- Frozen shoulder isn’t caused by cold weather, but symptoms may feel more pronounced during winter.
- It follows a predictable pattern of pain, stiffness and recovery can take up to 1 – 3 years without treatment.
- Hydrodistension and well-timed physiotherapy offer some of the best evidence-backed outcomes, significantly reducing recovery time.
- At London Bridge Orthopaedics, conservative treatment is always the first line of management, with surgery reserved for persistent cases.
What Exactly Is Frozen Shoulder?
Frozen shoulder develops when the capsule surrounding the shoulder joint becomes inflamed and stiff, limiting movement and causing pain. The exact cause isn’t always clear, but there are well-recognised triggers and risk factors.
Key Risk Factors Include:
- Diabetes – Up to 30% of affected individuals have diabetes, and diabetics are five times more likely to develop frozen shoulder than the general population.
- Thyroid disease
- Previous shoulder trauma or surgery in that arm
- Previous frozen shoulder in the other arm
- Autoimmune disorders
- Prolonged immobilisation (e.g., after fracture or dislocation)
- Post-vaccination – seen after Flu vaccinations and more common with increased Covid vaccinations following the Covid Pandemic
Frozen shoulder typically affects people aged 40–65, with women affected slightly more often than men.
How Common Is It?
Frozen shoulder affects approximately 2 – 5% of the population, but in those with diabetes incidence may rise as high as 20 – 30%.
Many patients experience symptoms for months or even years, and without treatment, recovery can be slow.
Is Cold Weather to Blame?
There is no evidence that frozen shoulder develops because of colder weather or winter. However, colder temperatures can make symptoms feel more intense because:
- Muscles and tissues naturally stiffen when cold
- Pain perception may increase with temperature change
- Reduced activity in winter means joints may stiffen faster
So while winter doesn’t cause frozen shoulder, it may make an existing condition more noticeable or harder to tolerate, which is why January and February are often our busiest months for assessment.
The Three Stages of Frozen Shoulder
Most patients progress through three recognisable stages, though the timeline varies:
Freezing Stage (Painful Phase)
- Persistent, deep pain
- Gradual, noticeable loss of movement
- Can last 2 – 9 months
Frozen Stage (Stiff but Less Painful Phase)
- Movement significantly restricted
- Pain may lessen, but function is impaired
- Typically 4 – 12 months
Thawing Stage (Recovery Phase)
- Slow return of range of motion
- Can take 6 – 24 months
Without treatment, full recovery may take up to 2 – 3 years and some individuals never regain complete mobility.
Diagnosing Frozen Shoulder
When you come to an appointment at London Bridge Orthopaedics, the first thing that your specialist will do is take a detailed history of your injury and symptoms. They will also carry out a clinical assessment of your shoulder, looking at your movement, strength and function.
With a frozen shoulder there are very classic symptoms and restricted movement patterns that will guide your diagnosis.
Because of this diagnosis is very straightforwards, and is largely based on:
- History (onset, pain pattern, functional loss)
- Physical examination (notably restriction in both active and passive movement)
Imaging such as X-rays or MRI are only really used to exclude other conditions such as rotator cuff tears or arthritis, but the hallmark remains a physical assessment showing global restriction of shoulder movement with pain at end ranges.
Treatment: Why Timing Matters
The approach to treatment depends significantly on which phase of frozen shoulder the patient is in.
At London Bridge Orthopaedics, we always begin with conservative management, focusing on reducing pain, improving mobility, and supporting recovery.
Treatment Pathways Include:
Early Stage (Painful Phase): Symptom Control
- Pain management (simple analgesia, anti-inflammatories if tolerated)
- Targeted physiotherapy focused on gentle mobility
During this stage, aggressive stretching often increases pain, so a measured approach is essential.
Hydrodistension: A Key Turning Point
One of the most effective interventions, particularly during the frozen phase, is hydrodistension (also known as capsular distension).
This minimally invasive procedure involves:
- Injecting saline (salt water), with local anaesthetic and sometimes corticosteroid into the shoulder joint
- Gradually expanding the joint capsule
- Breaking the adhesions mechanically and chemically
Hydrodistension can:
- Reduce pain rapidly
- Restore mobility
- Accelerate progression into the recovery stage
- Improve physiotherapy outcomes
Many patients notice improvement within days to weeks, especially when followed by structured rehabilitation.
Physiotherapy: Correct Dose at the Right Time
Physiotherapy remains a cornerstone of recovery – but it must be timed appropriately.
| Phase |
Aim of Physio |
Approach |
| Painful Stage |
Settle symptoms |
Gentle, pain-free mobility only |
| Frozen Stage |
Regain movement |
Gradual stretching and capsular mobilisation |
| Thawing Stage |
Restore normal function |
Strengthening and functional retraining |
Working with a physiotherapist familiar with frozen shoulder is important, to avoid overloading the joint and prolonging pain.
At London Bridge Orthopaedics we work with highly experienced and trusted Physios who will ensure you receive the best treatment.
When Is Surgery Considered?
Surgery is rarely required. However, if symptoms remain debilitating after 6 – 9 months of conservative therapy, the following procedures may be considered:
Both aim to restore motion by releasing the contracted capsule, and are usually followed by immediate physiotherapy to maintain gains.
Prognosis: What Can Patients Expect?
With appropriate management, the majority of patients achieve:
- Good to excellent long-term function
- Significant reduction or complete resolution of pain
Hydrodistension and evidence-based rehabilitation can shorten recovery, compared with natural progression.
However, patients with diabetes may have:
- A slower recovery trajectory
- A slightly higher recurrence rate
- Persistent mild stiffness compared to non-diabetic individuals
Early diagnosis and personalised treatment significantly improve outcomes.
Summary
Frozen shoulder can be extremely frustrating; everyday tasks such as fastening clothing, reaching overhead, or sleeping can become a challenge. But with well timed intervention, structured rehabilitation and the right clinical guidance, recovery is not only possible, but it can be significantly accelerated.
If you are experiencing shoulder stiffness or persistent pain this winter, a clinical assessment can help determine whether you’re in the early freezing stage or further along, and we will guide you toward the most effective next step.
Frequently Asked Questions (Q&A)
What is frozen shoulder?
Frozen shoulder, or adhesive capsulitis, is a condition where the shoulder capsule becomes thickened, inflamed and stiff, leading to restricted movement and shoulder pain. It typically develops gradually and may progress through defined stages before improving.
Does cold weather cause frozen shoulder?
No — cold weather does not cause frozen shoulder. However, low temperatures can make stiff joints feel more uncomfortable and may increase awareness of symptoms, which is why many people report worsening during winter.
Who is most at risk of developing a frozen shoulder?
Frozen shoulder is most common in adults aged 40–65. Individuals with diabetes, thyroid disease, autoimmune conditions, recent immunisation, or a history of shoulder injury or surgery are at higher risk.
How is frozen shoulder diagnosed?
Diagnosis is primarily clinical, based on symptoms and reduced both active and passive range of motion. Imaging such as X-rays or MRI can help rule out other shoulder conditions such as arthritis or a rotator cuff tear.
What is hydrodistension and how does it help with frozen shoulder?
Hydrodistension is a minimally invasive procedure where fluid is injected into the shoulder joint to gently stretch and expand the tight capsule. This can help improve movement, reduce pain and accelerate progression into the recovery stage. It is often combined with physiotherapy.
Do I need surgery for frozen shoulder?
Most patients recover without surgery. At London Bridge Orthopaedics, conservative management — including pain control, physiotherapy and hydrodistension— is always the first-line approach. Surgery is reserved for cases where symptoms remain severe and function remains limited after several months.
How long does frozen shoulder take to recover?
Without treatment, frozen shoulder may take 1–3 years to fully resolve. With targeted intervention such as hydrodistension and physiotherapy, recovery time can be significantly reduced.
Can frozen shoulder return after treatment?
Recurrence is rare, though individuals with diabetes have a slightly higher chance of residual stiffness or recurring symptoms.
Useful links:
https://www.nhs.uk/conditions/frozen-shoulder/